Design for Telehealth
Growing Access to Long Distance Medicine
Moving through the Welcome to Telehealth kit, the first product design output for the Telehealth project. Here is a link to the prototype kit.
Moving through the Telehealth Toolkit, the second product design output for the Telehealth project. The prototype kit is no longer available, but you can read about it below or here on the wiki for project.
Service design output for the Telehealth project: an Editorial Board kickoff meeting for the Telehealth Toolkit Knowledge Management Tool.
Project Duration: In stages, 1 year. Status: Implemented
Project Type: Federal
Agency Partner: Veterans Experience Office (VEO), Office of Telehealth (Telehealth), both, Department of Veterans Affairs
Role: Lead
Stakeholders: Telehealth, Veterans, Caregivers
Design Phases: Research, Design, Implementation, Measurement
Skills: Strategy, Research, Product, Service, & UX Design, Frontend Development
Implementation: In pilot, the Welcome to Telehealth kit increased the number of veterans able to successfully complete their first Telehealth appointment by 25% and reduced the number of veterans requesting additional information after being introduced to Telehealth from 75% to 14%, a 61% decrease.
Background
The Department of Veterans Affairs has the largest and most sophisticated long distance medical infrastructures in the world. Through the Office of Telehealth (Telehealth), a veteran living in rural Texas, for example, can see a specialist residing in Boston for consultation. In addition to mental health appointments, which seem a natural fit for long distance medicine, veterans can have blood drawn, get dermatological and optical scans, and other procedures performed at local clinics and then have the far away specialist consult with them face-to-face over video connections to learn their results and the next steps in their treatment. Through daily health screenings involving blood pressure monitoring and diet and exercise coaching, VA has been able to reverse diabetes. Reverse! I didn't even know that possible.
But Telehealth had a problem: not that many people use the system, relative to the number that could. Veterans didn't seem to talk about Telehealth, and providers seemed to think that adding the Telehealth modality of care in addition to their tradition, in-person modality, would result in lower-quality care. This frustrated the Office of Telehealth leadership so that, during the Winter of 2017, they approached the Veterans Experience Office (VEO with an incredibly broad problem: how to get more veterans to use Telehealth as their healtcare modality? The VEO team immediately brought me on from the Lab team to head up the scoping and research for the project.
After initial project scoping talks, members from the Telehealth and VEO teams and I determined that Project Manager Lori Baca and I would lead a team of contractors and Telehealth staff people in open-ended, HCD research. We would then use that research as the basis for updating Telehealth's survey questions as well as for product or service designs that would help the Office increase use of its services across the veteran population.
Research
Research took place across 6 VAs in different areas of the country, including Sioux Falls, SD, Palo Alto, CA, and San Antonio, TX. We both visited and held virtual meetings with veterans and caregivers who had differing knowledge of Telehealth, as well as non-clinical staff, nurses, doctors, and administrators in the Telehealth system.
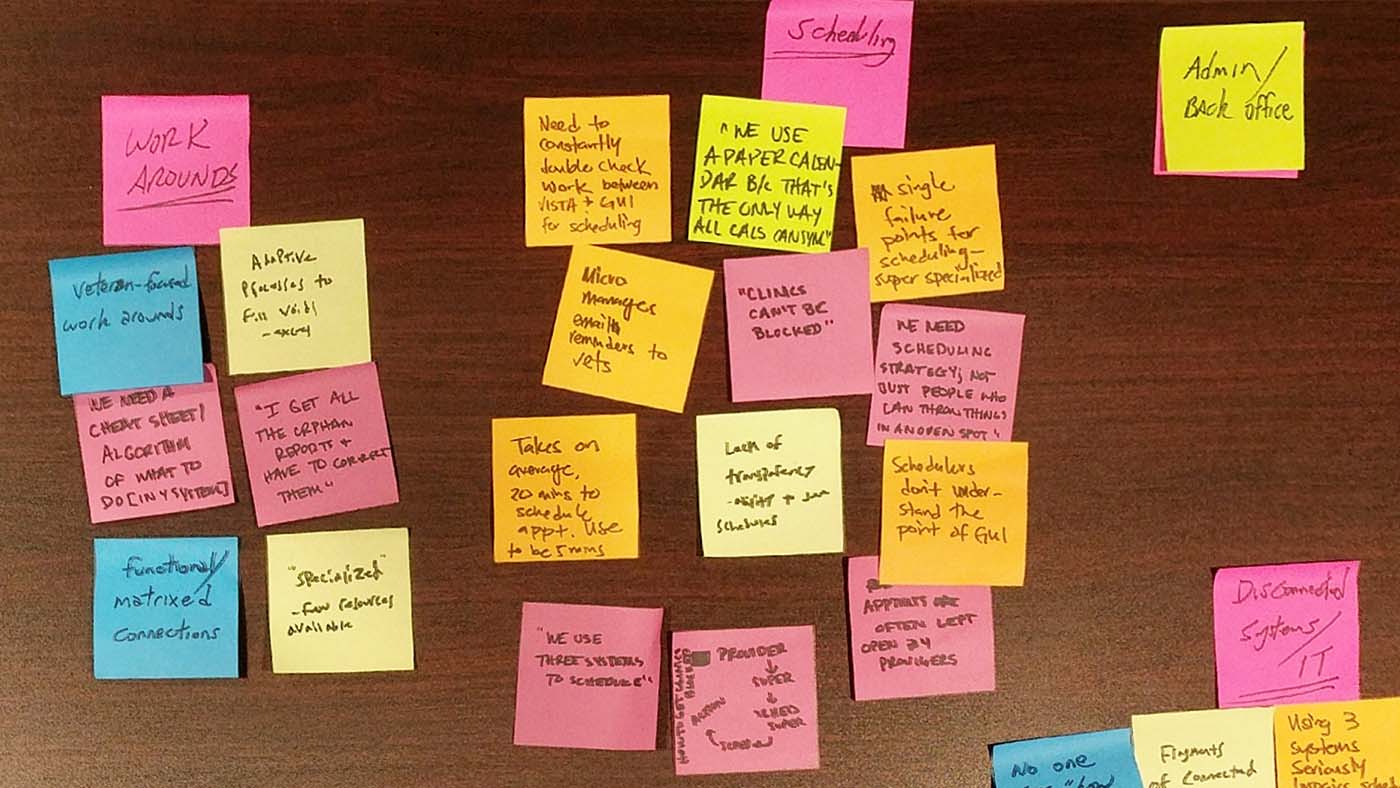
No Technical Solutions
In tackling this research, I think most of us believed there might be a technical solution: the gear that the veterans had to deal with would be fiddlely or prone to breakage, or the scheduling might be a software issue we could take on. Neither of those proved to be true. The hardware that the veterans use to send in their blood pressure and other readings worked very well. In fact, we didn't find any veterans who struggled with it. On the other hand, the scheduling system did prove to be a stumbling block for the staff, but Telehealth was already working on a solution, so we didn't pursue that avenue.
One technical contradiction between the veteran and Telehealth stakeholders did emerge early on, however: the requirement or ban of printed Telehealth materials. The Office of Telehealth is, after all, long distance medicine on the internet. They were quite rightly not particularly interested in printing materials: their services are by nature digital, and print assets are tough to update across a vast system. Veterans, on the other hand, told us over and over again that they would really like some printed directions about Telehealth. They wanted "something to hold on to...to put on my fridge when I get home." That was an interesting tension between the service providers and end participants. We filed it away to address during the Design Phase.
Research Synthesis
At the close of our research period (~4 months from start to finish), we found through our synthesis that we had two rich opportunity areas in which to design.
- Veterans had to be persuaded to use Telehealth. The idea that they would see doctors over the internet just did not sit naturally with many of them. This wasn't just a problem with older veterans; younger veterans and/or people living with PTSD or other disorders felt the modality might challenge them. They were reluctant. For this reason, Telehealth nurses who make up the majority of Telehealth staff at the time spent a self-reported average of 10 minutes doing what they called "selling Telehealth". Across multiple veteran appointments per week, that "sales" time was not only out of scope for a nurse's skillset, it also took away precious time they could be providing care.
- Doctors also seemed reluctant to convert some of their appointments to Telehealth. They perceived the system as inconsistent, or not in-keeping with the full scope of their medical practice. Again, the lift of persuading and support came from the Telehealth staff people. Only where the Telehealth staff was organized to pick up any issue as soon as it emerged was there high uptake and success in for Telehealth from providers.
After discussing it with Telehealth leadership, we decided we would focus first on a veteran-facing design solution and then double back for a bit more research on the provider side to support the onboarding of new providers. After all, if we were successful in bringing on more veterans to use Telehealth but there weren't enough providers, then the long wait times for appointments would do no one any good.
Welcome to Telehealth Kit
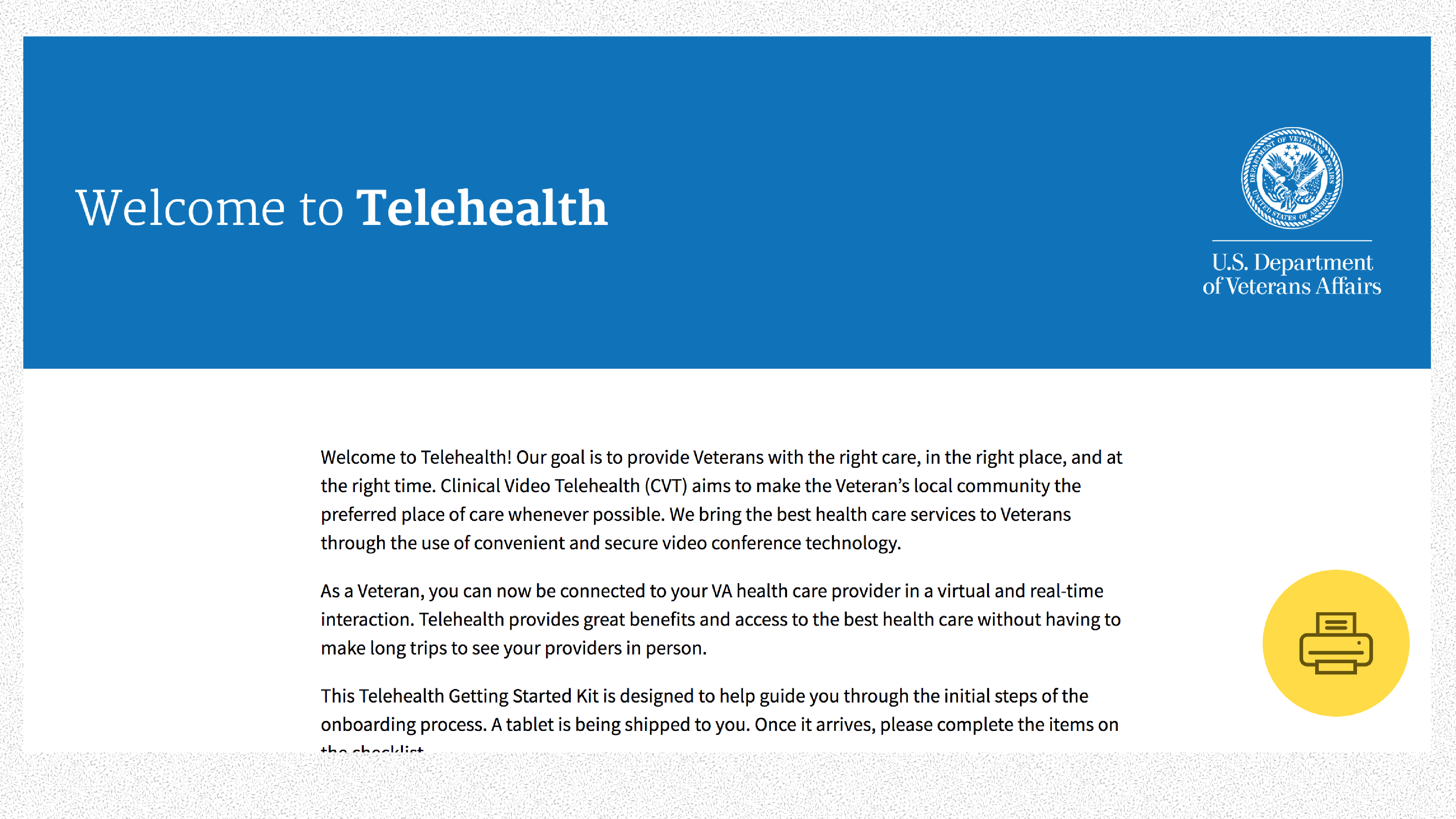
The Welcome to Telehealth Kit was the first product we realized from the Telehealth research. We focused in on the core problem outlined in point 1, above: how to make veterans feel more comfortable trying the Telehealth care modality, and how to reduce the time nurses had to spend "selling" the service. Here is a link to interact with the prototype Kit, but please note, this prototype is no longer supported for all compatibility across all browsers.
Concept
As the Lead Designer, I ran through these "sales" moments over and over. Along with the team, we evolved the idea of providing the nurses with a small "gift" to give the veterans when they made their first appointment; something they could hold on to and take home. We centered it around the idea of the small samples of makeup one gets at the beauty counter; they aren't big, but they're beautiful and show you just enough of the products to make you feel like you can try them. While that framing was met with some doubt by Telehealth leadership, they let us go ahead.
The opening screens of the Welcome to Telehealth Kit focus on a welcome and completing your first appointment
Content
Editorially, we tested the content with veterans over and over again to get just the right amount of information. In the end, the Kit doesn't really spend a lot of time "providing directions" on troublehshooting; the first thing it says is to simply call the Telehealth Helpdesk if you have any problems with your technology.
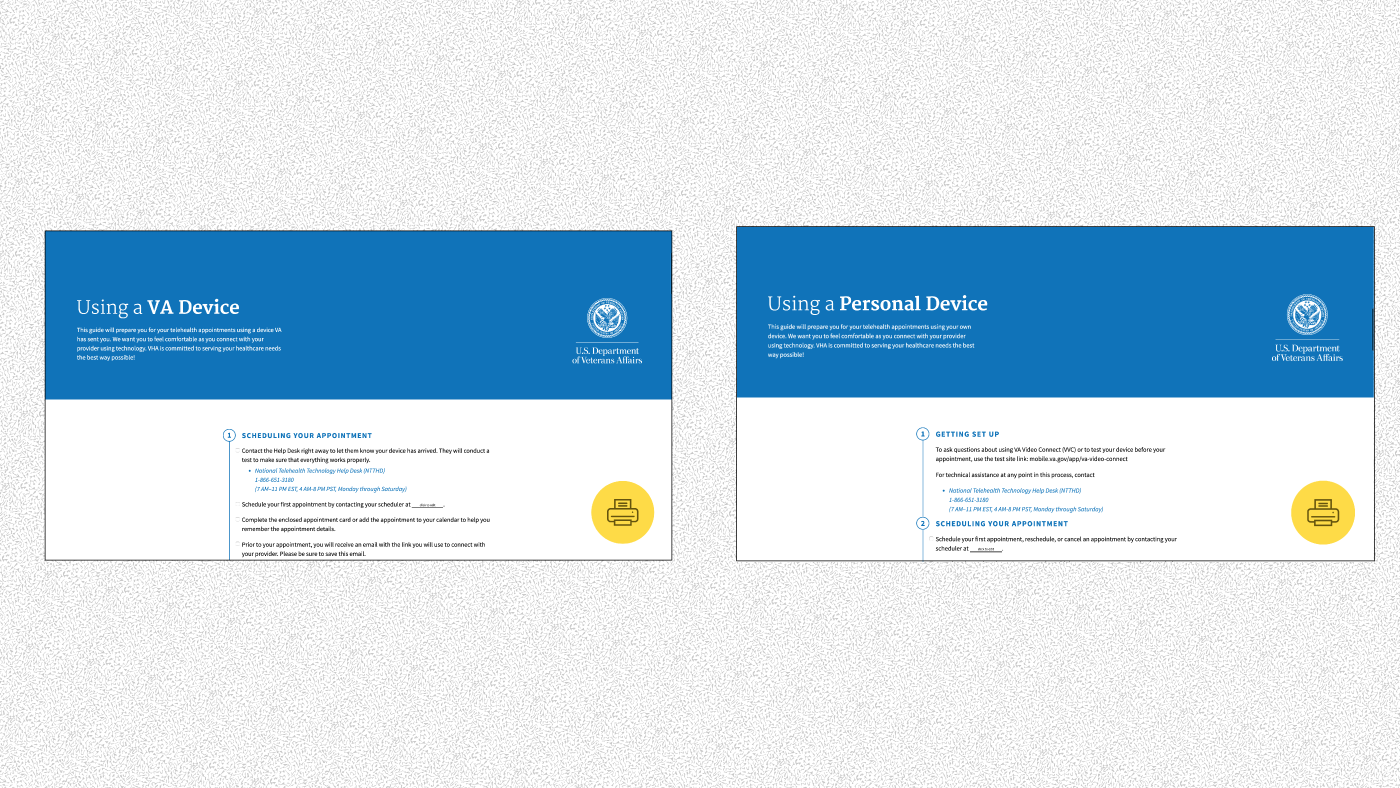
VA will either issue a veteran a tablet or phone to use the Telehealth service or the veteran can download secure software and use their own equipment.
Instead, the Kit's contents focuses on giving the veteran wrap-around service: the blanks can be filled in by the nurses either on their computers to print or with pens in person to let the veterans know the names of contact people, the locations for technology return, and other information pertinent to the individual.
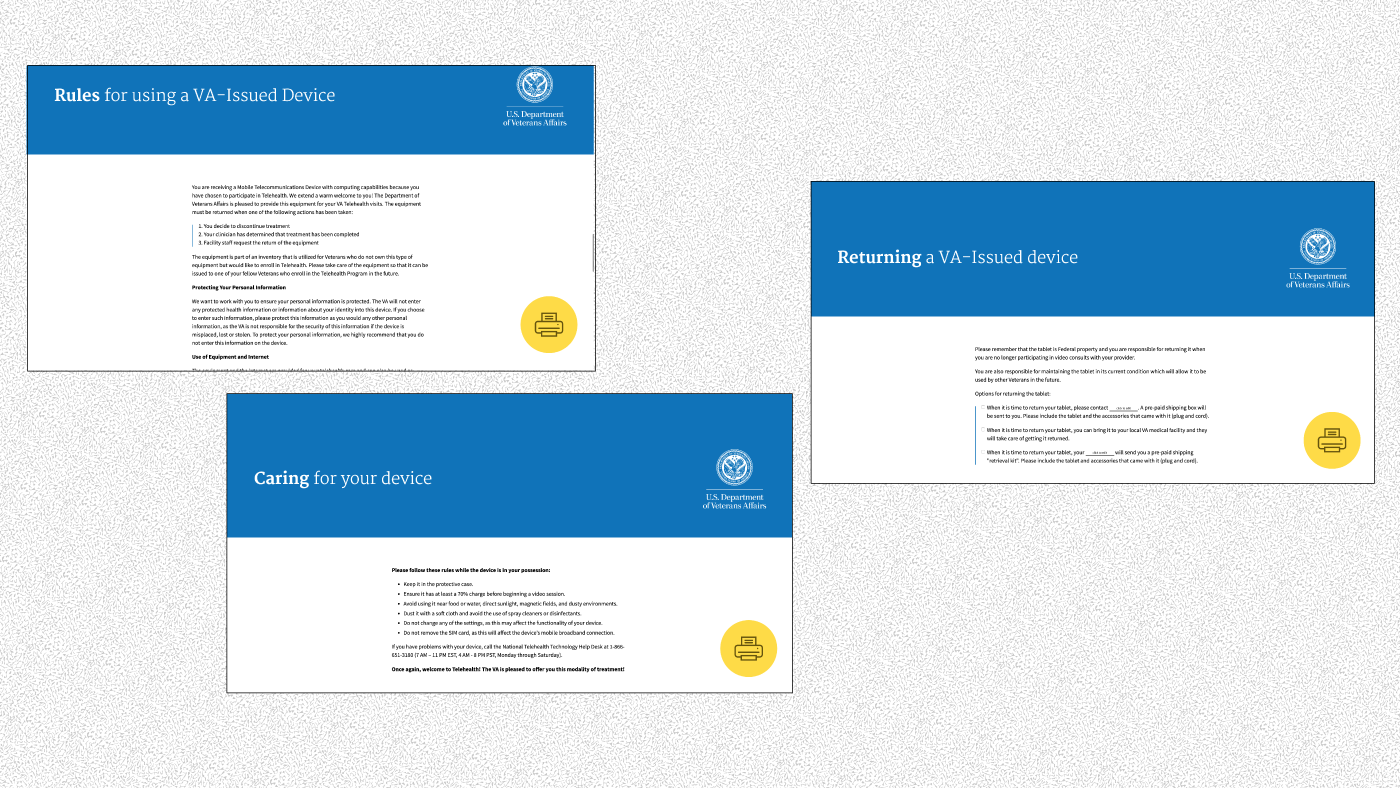
Interestingly, the language on these three screens required repeated conversations with Telehealth. We need to inform the veterans of their responsibility, but not make it sound putative or harsh. Getting this language to ring just right required many iterations and tests.
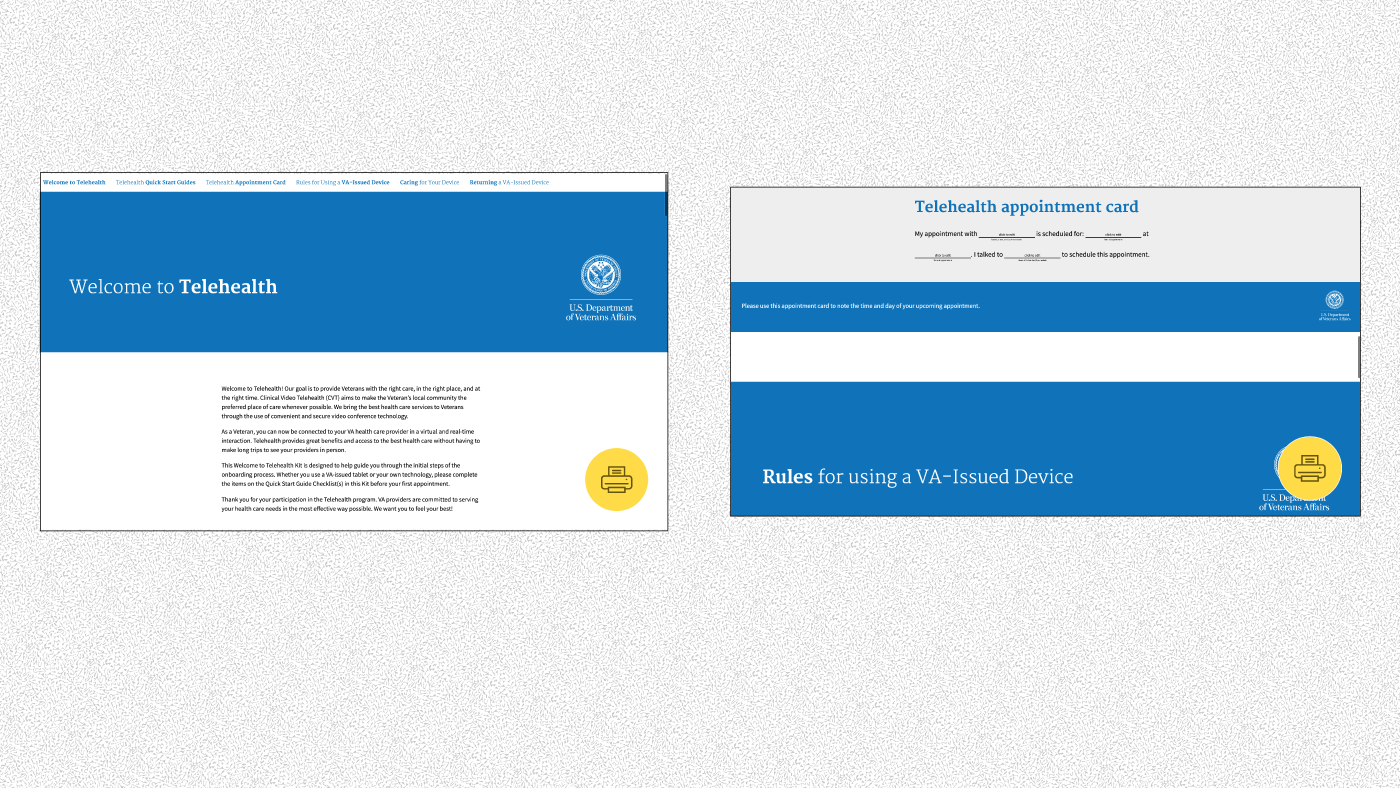
Form
The veteran-facing form for the Welcome to Telehealth Kit is almost a copy of the Welcome Kit, a 2018-launched product for service people transitioning from military to veteran status. Researched extensively by the VEO team through 2016, we knew the form worked for veterans and caregivers. Plus, since it had recently launched nationwide, we knew that its form would be familiar to any new veterans approaching Telehealth.
One problem: the Welcome Kit is print-only. And the Office of Telehealth, as I said above, would not do print runs. But on the other hand, veterans had told us that they would like printed materials. So we had to find a solution.
Having learned design largely on the job in the photography and motion picture worlds, I know the power of a beautiful, considered, flawless final product. That's what I wanted for the Welcome to Telehealth Kit: that anyone who interacted with it, in print or digital, would feel like they were considered and that their experience was important to someone, whoever designed that thing they have in their hands.
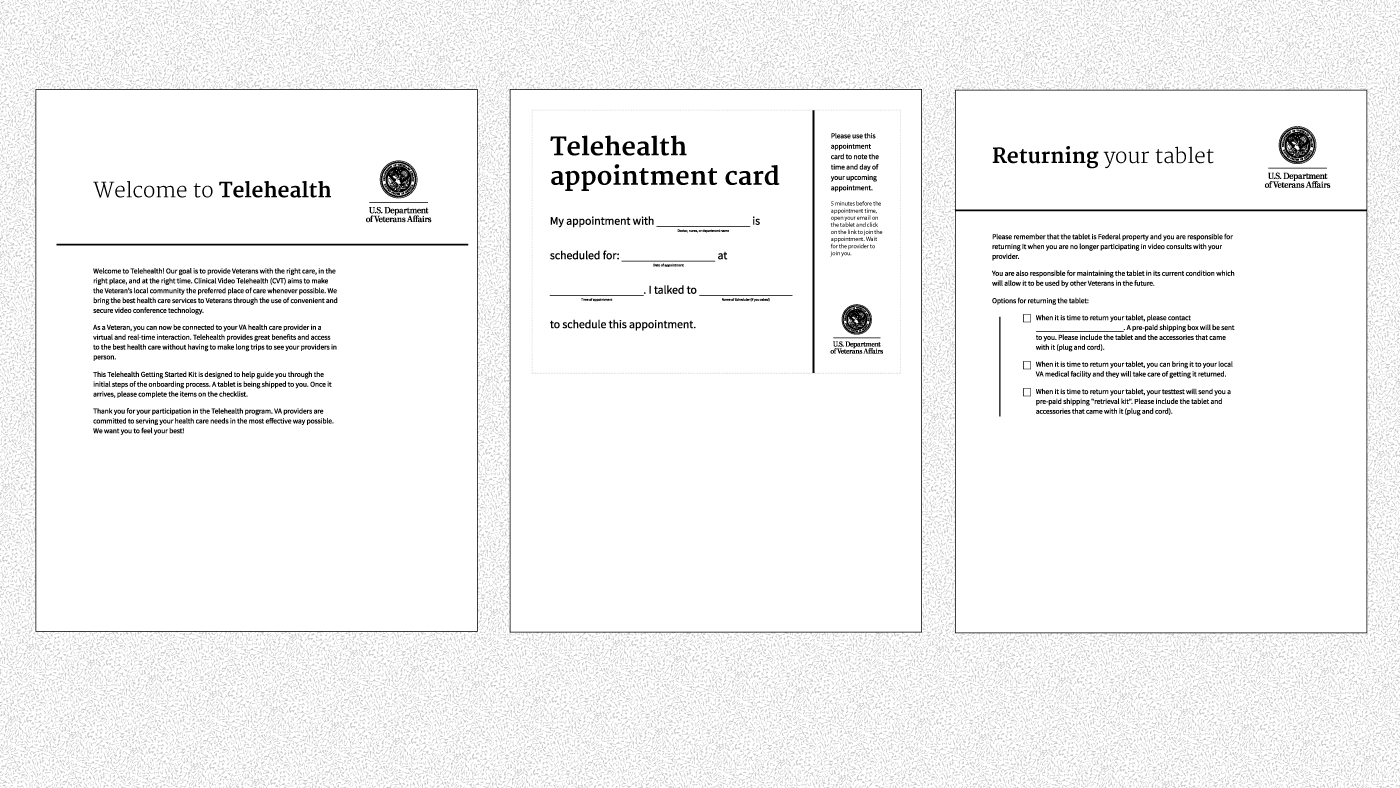
So we pushed an old technology, print media tags, in a deeply intentional way and some majorly elegant CSS, we were able create this beautiful, meaningful Welcome to Telehealth Kit that lives in digital, but prints in a clean, easy-to-read black and white layout. The black and white was important as well, since we learned halfway through iterations that almost none of the VA Medical Centers allow color printing; it's too expensive. So another CSS trick was deployed to create the single color layout. In a wonderful way, the emotional and technical solutions for our problem combined in this simple, clean website.
Supporting the Telehealth Staff
In the course of iterating on the Kit itself, Telehealth staff people started asking for additional support so they could implement the Kit effectively.
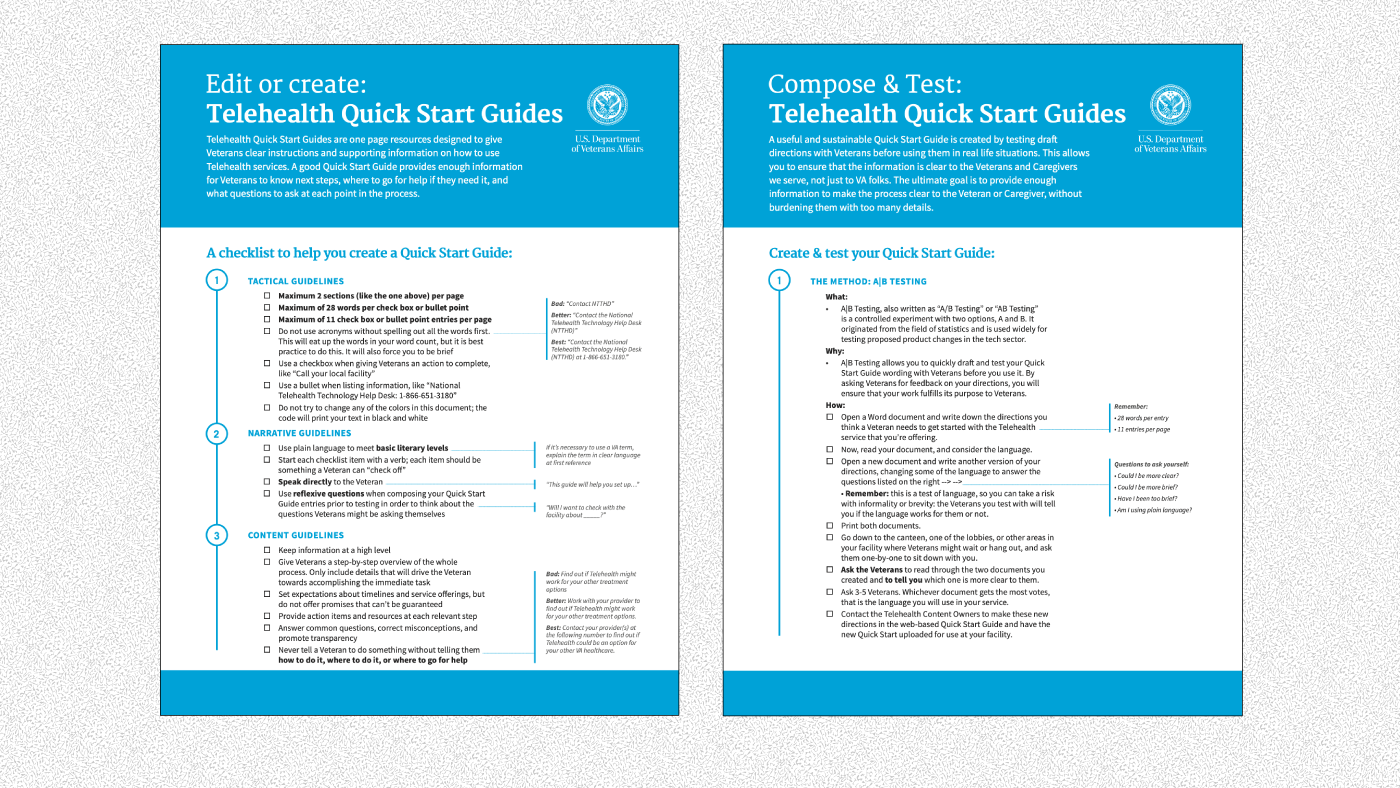
These included documentation on A|B testing language, so they could update it as technology and policy changes and an introductory script to use. The latter request surprised me; I thought it was too heavy-handed to tell these sophisticated healthcare providers what to do, but to my surprise, the script tested well, and people requested its inclusion in the formal Kit pilot.
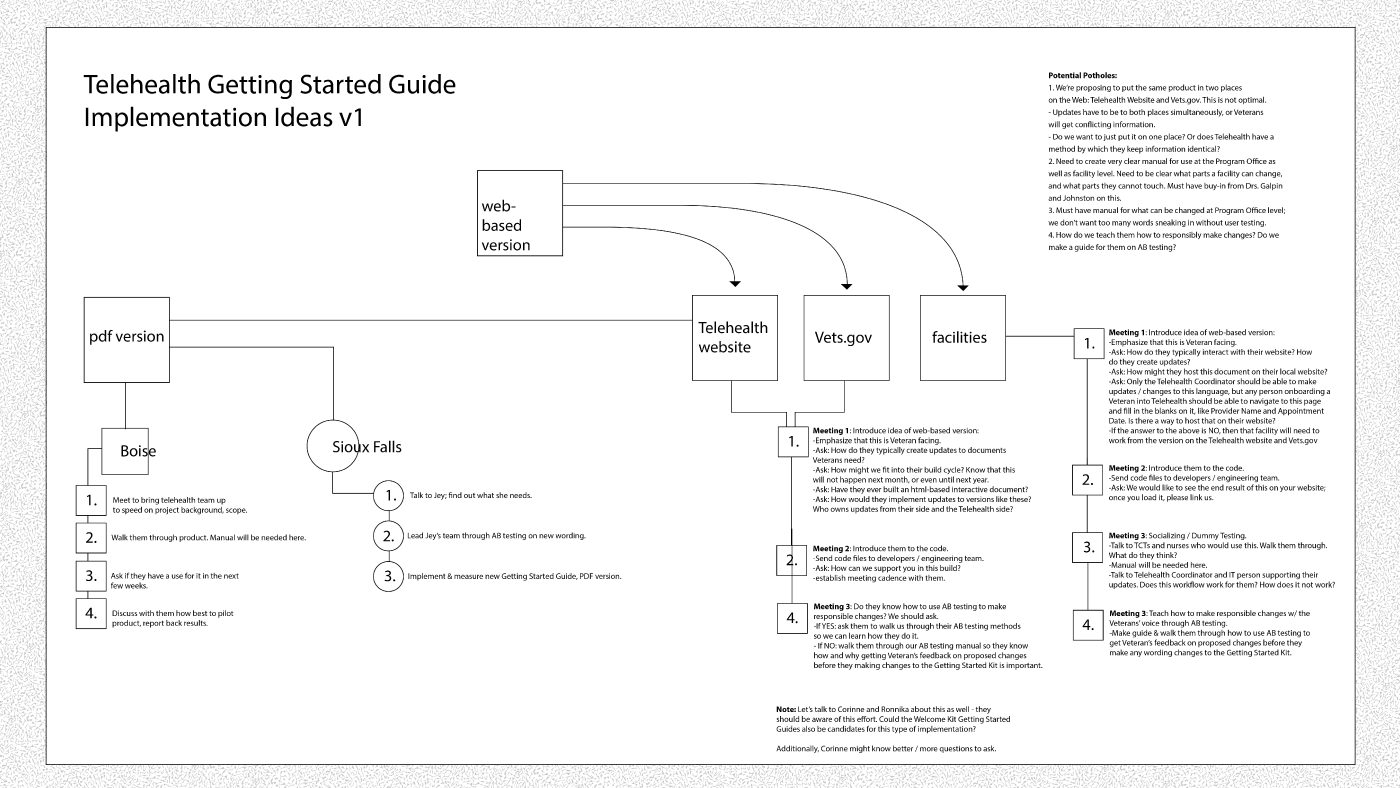
Implementation plan for Welcome to Telehealth Kit pilot sites. We were aware that the multi-stakeholder nature of the Kit would slow implementation. For this reason, we focused on the VA Medical Centers as our primary pilot sites so we could get the positive use numbers from healthcare providers behind the product before approaching the administrative stakeholders.
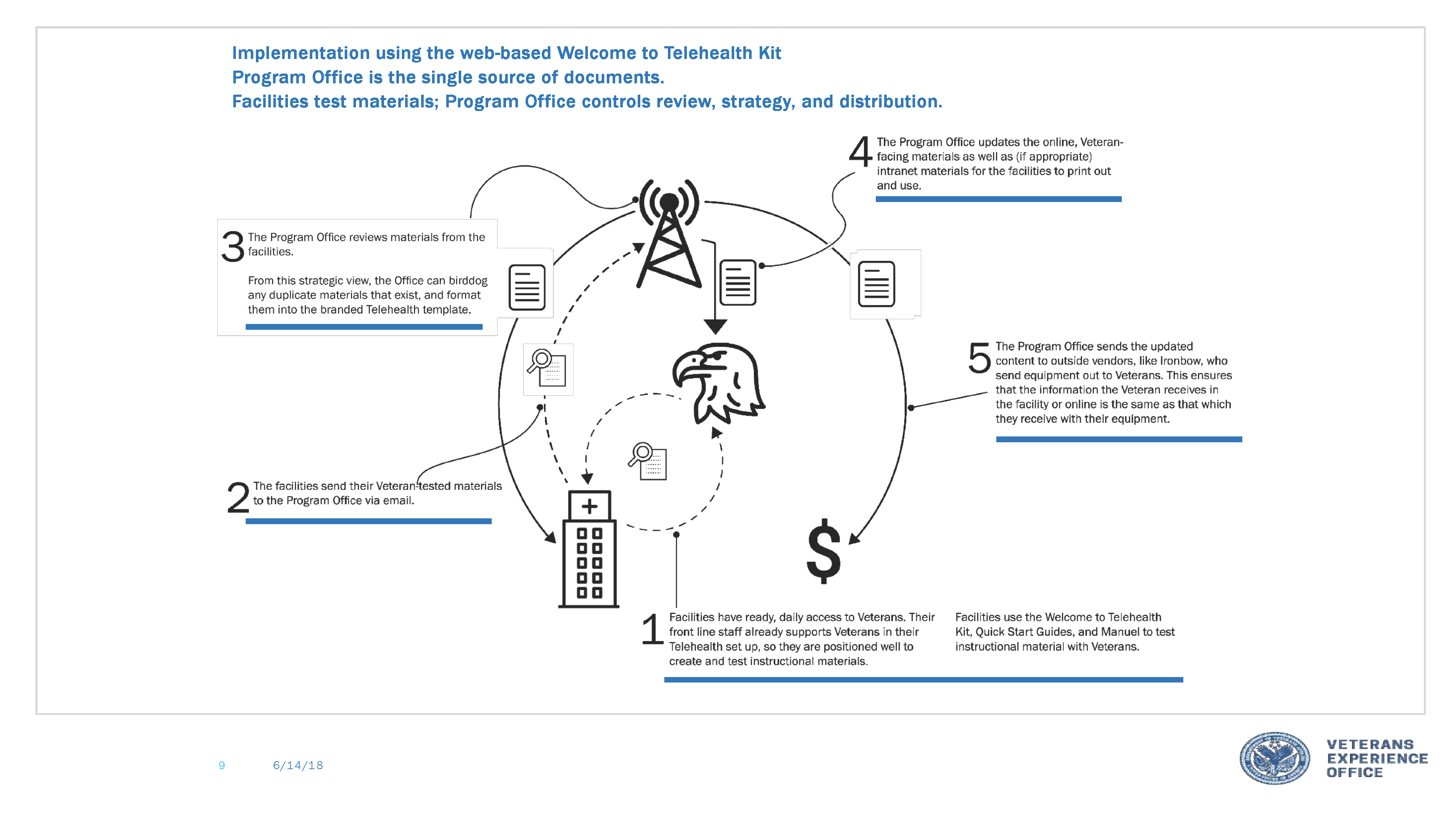
The higher-level, conceptual basis for this implementation plan. The Medical Centers must pilot the Welcome Kit, as they have ready access to veterans. They can personalize the kit to a certain extent, but not completely. For more strategic changes, they would need to work with the Telehealth program office to affect the base code.
Pilot Results
Although the sample sizes are small across two Telehealth sites in different states, the data demonstrates the Welcome to Telehealth Kit, if applied as it was designed, has the potential to make a significant impact in improving the veteran's experience and the use of medical facility resources. Qualitative Data we gathered in pilot indicate:
- Patients don't have to listen so intently or try to take notes as they know they will be taking written information home, which provides a sense of security.
- Patients agree to sign up for Telehealth more readily once the Kit is presented, alleviating the staff from "selling" Telehealth.
- A 25% increase in the number of veterans able to successfully complete their first Telehealth appointment.
- A reduction in the number of veterans requesting additional information after being introduced to Telehealth from 75% to 14%, a 61% decrease.
Future Welecome to Telehealth Kits
Several Telehealth staff recognized that the Welcome to Telehealth Kit could be adapted and utilized for any Telehealth services that Veterans receive in the home. We are currently hearing more about its use and the potential to evolve the Welcome to Telehealth Kit in the near future.
Telehealth Toolkit
Click through of the prototype site for the Telehealth Toolkit. This was developed with the Office of Telehealth, Telehealth staff people, the Veterans Experience Office, and the Lab at OPM in the Summer and Fall of 2018. It was built in Angular using components from the U.S. Web Design System.
Background
Drawing on the qualitative research generated in the winter and summer of 2018, a VEO and Lab team developed the Telehealth Toolkit product for VHA's Office of Telehealth. Under the Office of Connected Care, the Office of Telehealth is responsible for providing long distance medical treatment in a variety of formats for veterans across the United States. Far outpacing its private, domestic competitors, the U.S. Department of Veterans Affairs currently operates one of the largest long distance medical services in the world. The Telehealth Toolkit development is in response to the VA agency goal of rapidly expanding the availability of the Telehealth across the final years of this decade.
Converting Providers to Telehealth
To support this expansion, the number of healthcare providers practicing the Telehealth modality of care will also need to be expanded. In studying how best to engage providers in this relatively new modality, however, the research team found that many providers are disinclined to practice Telehealth for a variety of reasons.
To convert providers to Telehealth, the facility Telehealth staff frequently embrace the role of full-service Telehealth support network: from scheduling to training to technical support, the staff are at the elbows of the providers to ensure the provider and veteran have a successful Telehealth experience in each appointment. Given this reality, the research team concluded that to empower providers to use Telehealth is to empower the Telehealth staff to support them. One of their major barriers: how to access guidance, support documentation, marketing materials, and subject matter experts for the entire Telehealth program.
A Combined Service and Product Design Project
The Telehealth Toolkit product consists of two parts:
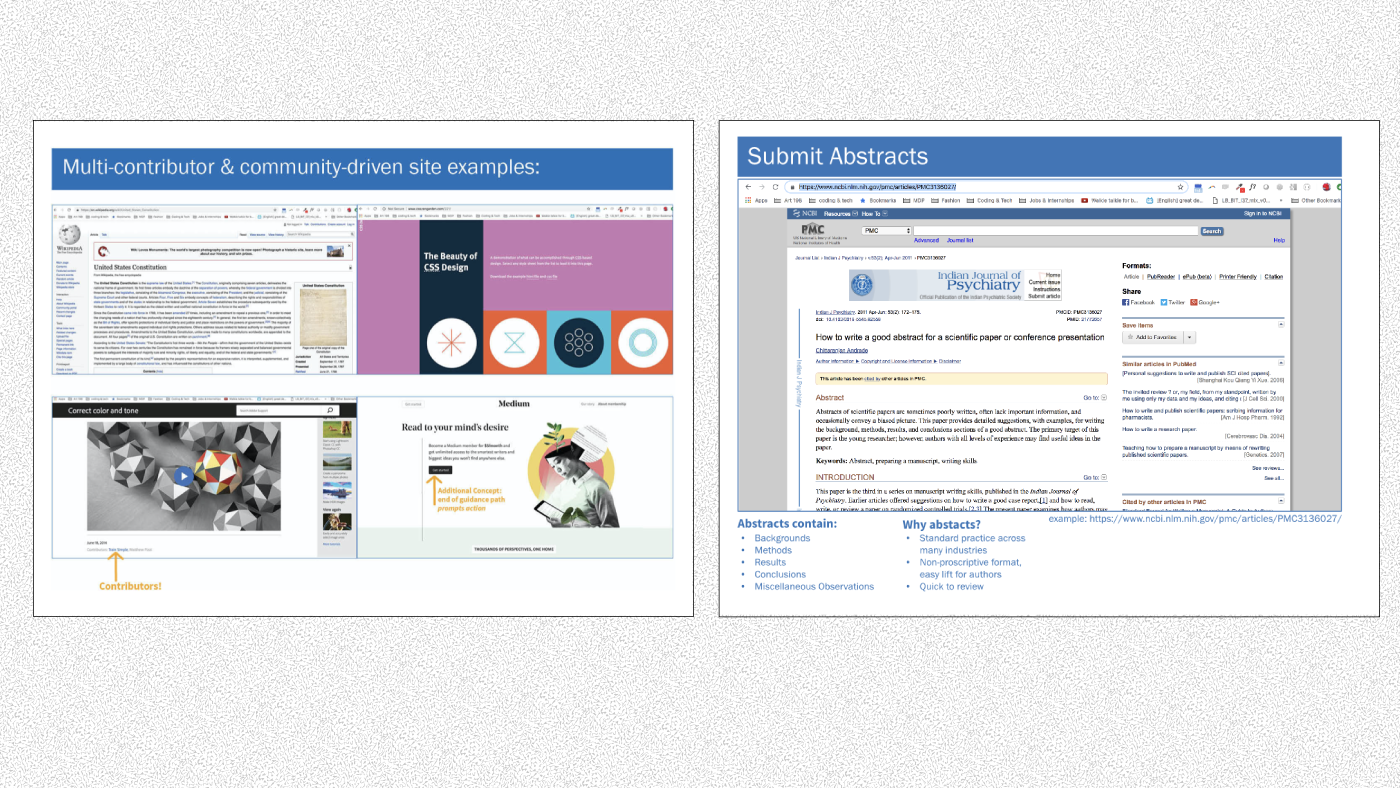
- A peer-contributed documentation website. Multi-contributor content generation is practiced in long-established industries such as magazine publishing and technology, while peer review is a common and well-respected method of knowledge sharing in the sciences. In this way, we could validate the efficacy of crowd-sourced knowledge sharing, while building the system of content creation inside a review mechanism well-known to our participants.
- An editorial workgroup that moderates the contributed content.
Product Design: the Telehealth Toolkit Website
From our research, we knew that the Toolkit's main purpose had to increase the accessibility of training and guidance documents for Telehealth staff. Its core goals included:
- Decreasing the time and energy staff spend searching for documents in the current organizational format.
- Decreasing the duplicative content generation efforts across sites.
- Increasing Program Office and facility-level collaboration around content generation and editing.
- Increasing cross-facility knowledge sharing.
- Increasing the visibility and accessibility of Telehealth to facility administration and service lines.
Inspired by the service provided by tech companies like Apple Computers, Telehealth leadership and the design team focused on the nature of the service provided by the Telehealth staff and how to systematize and support that service.
This was an interesting moment in our collaboration with the Office of Telehealth. The Genius Bar concept wasn't particularly well-suited to the service the nurses provide the doctors in Telehealth; the nurses come to the doctors (not the other way around), and the doctors aren't interested in learning about the minutae of Telehealth; they're interested in providing care. So unlike Apple's Genius Bar, this wasn't about providing the audience (the doctors) with an understanding of the system; this was about providing the Geniuses with connections to each other so they can trade knowledge across the entire Telehealth organization.
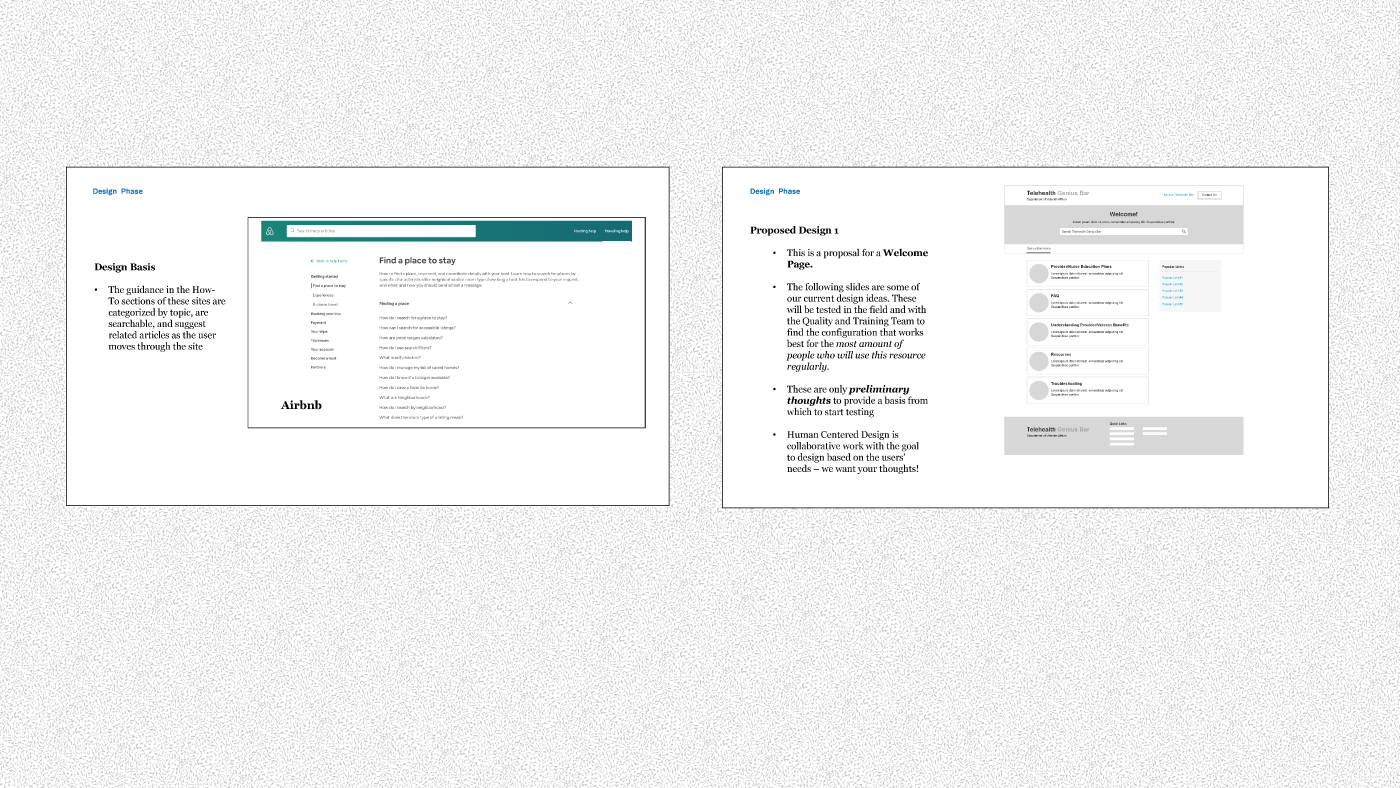
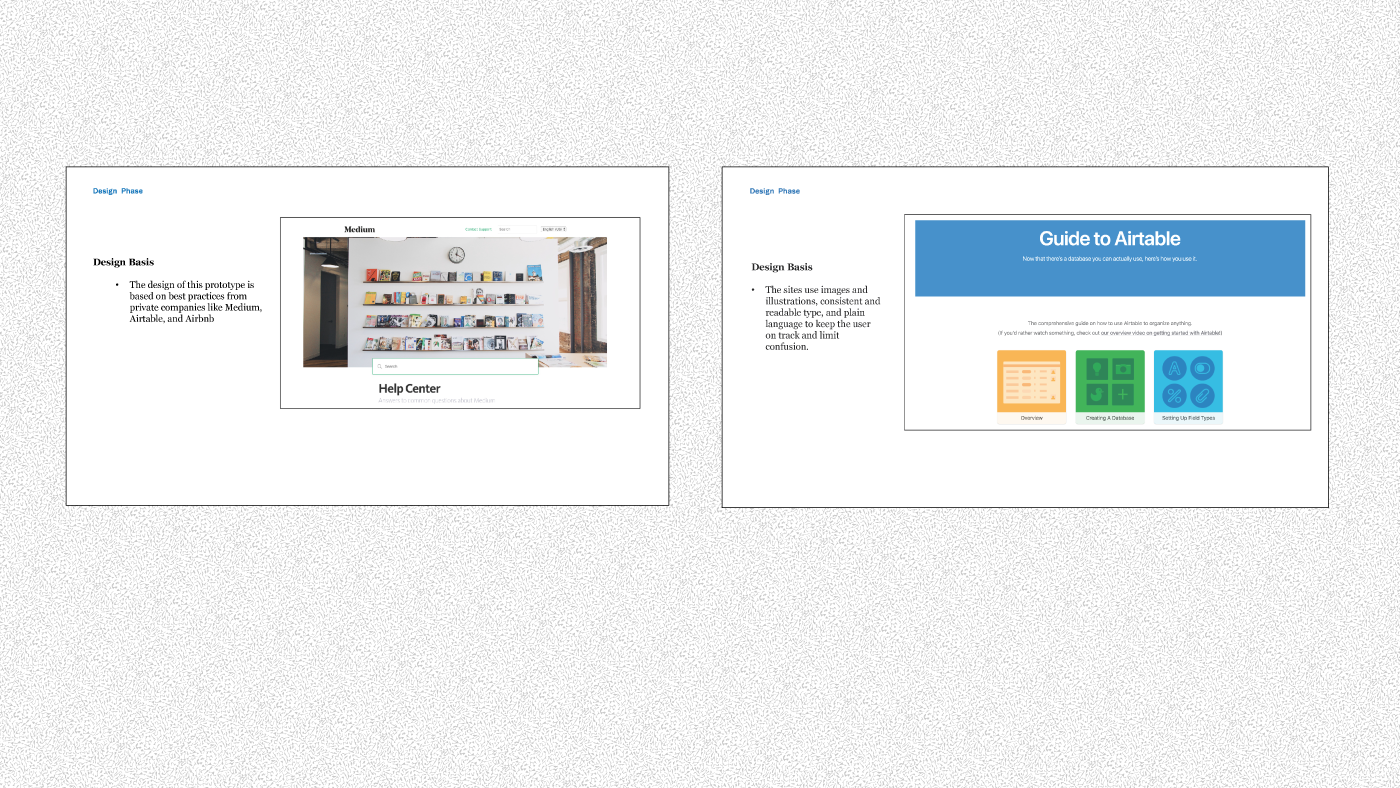
Since the nature of our work was to create a space for the Geniuses, aka the Telehealth staff people, to connect and share their methods, we knew we had to have a digital product. I pulled some references for robust, beautiful, active online communities to show to the Telehealth leadership. As you notice from the text, working to bring stakeholders sometimes means explicitly calling out the need for their feedback.
To encourage interaction, I knew we had to show stakeholders what pages could look like. VA doesn't have a consistently implemented style guide for their websites, nor is there any community like this in the VA system. So again, I pulled some references and explained what this site could be like.
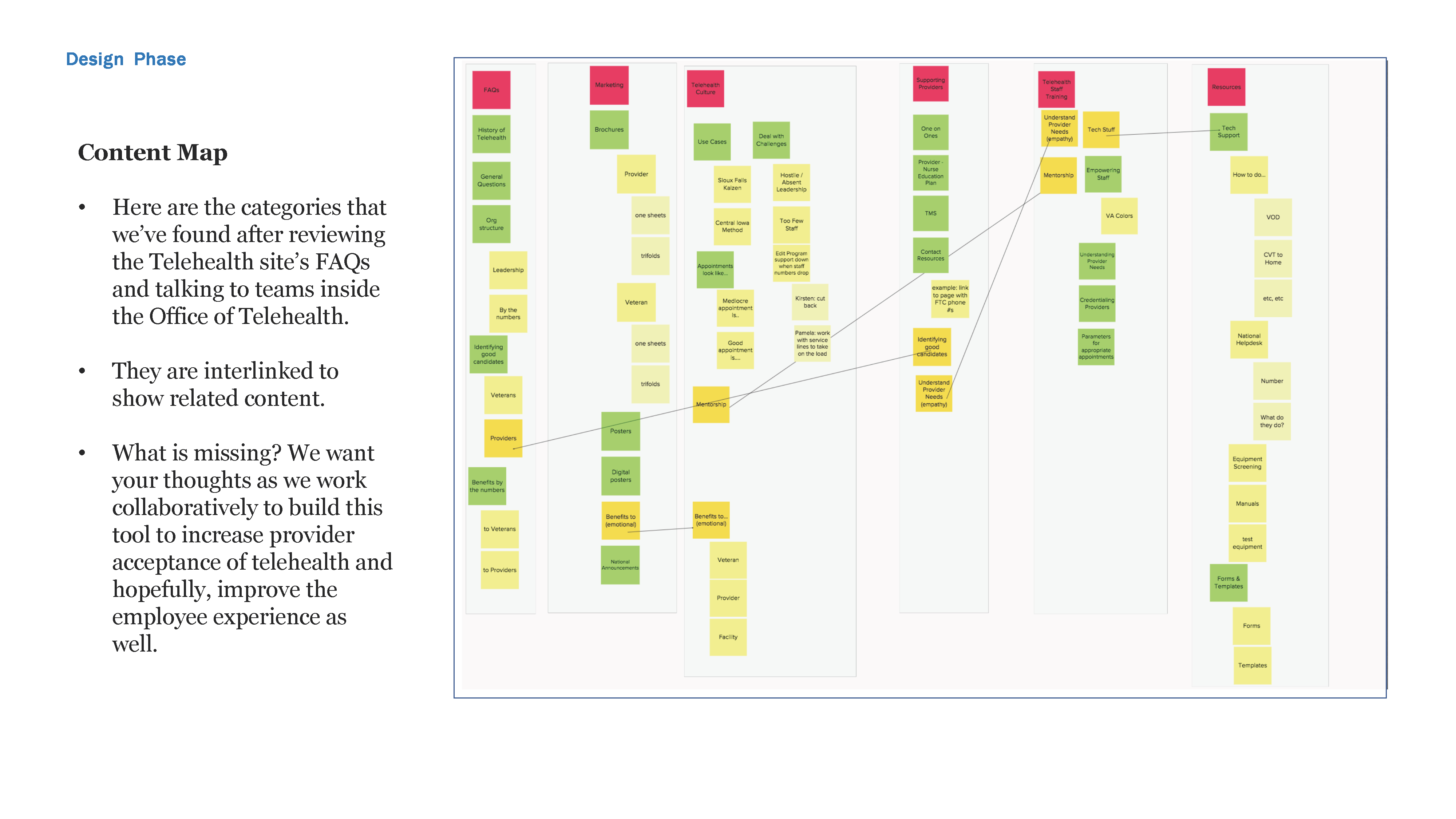
This content map came directly from our research in Summer 2018. We visited the VA Medical Center in Fargo, ND to form the bulk of this organization, then validated it virtually with other sites.
Service Design: the Editorial Working Group

In order to pull content for the Telehealth site, we worked with Telehealth to draw together an Editorial Working Group with members from all levels of the Office of Telehealth, from front line staff to senior leadership. We convened in Denver in October 2018 for our kickoff meeting. The workshops core goals included:
- Establish the workgroup and its mission.
- Map out the current process for content generation.
- Map out an ideal process for content generation.
- Generate next steps for the workgroup in terms of editorial and technical needs.
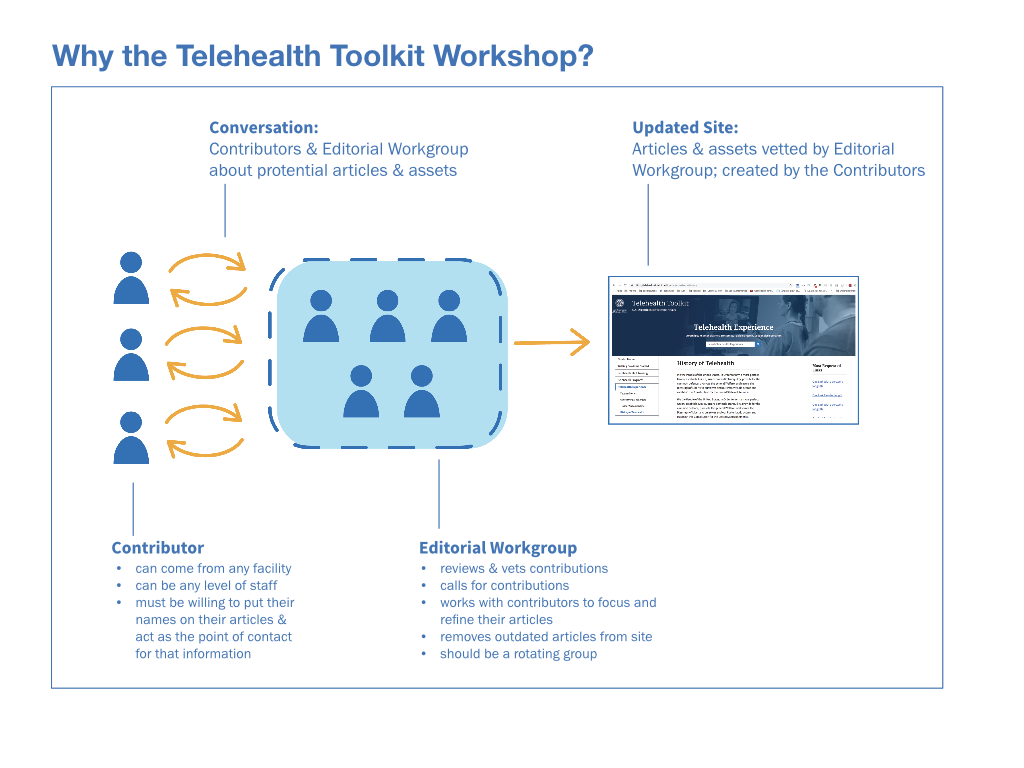
Building a Community of Contributors
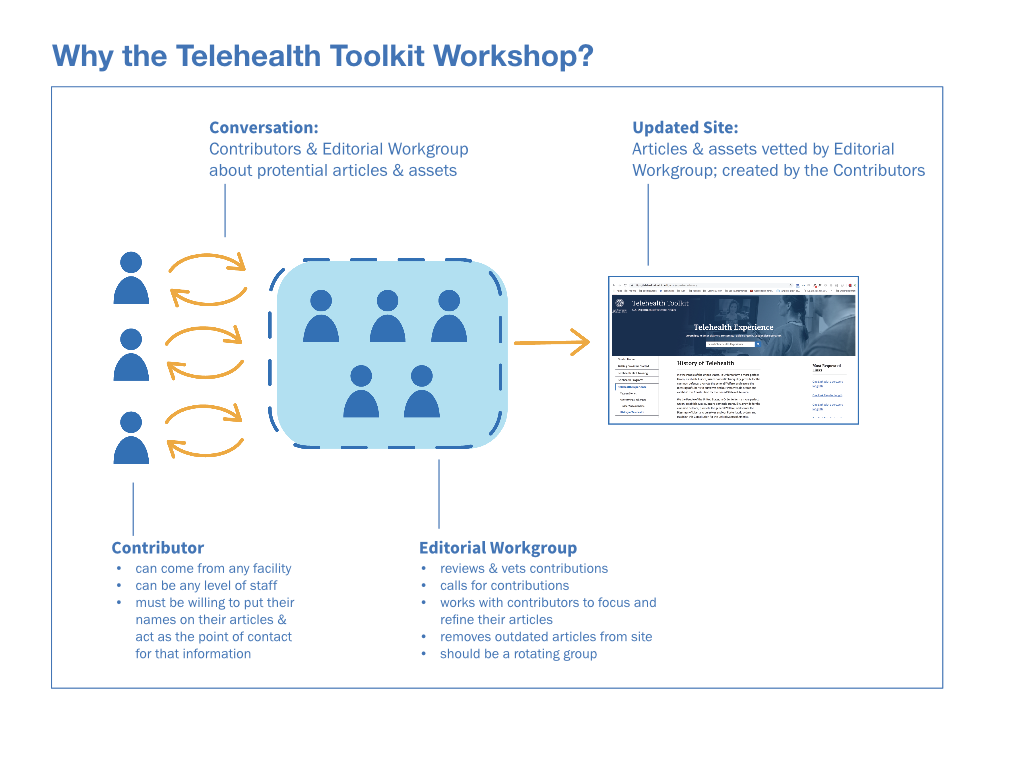
A central part of the Editorial Working Group was the building a community of contributors. A vibrant community of this type relies on a reliable and open culture of communication channel through which the Editorial Working Group and potential contributors can converse. Though not all contributions would be accepted, the community can be nurtured through the careful administration of critique, encouragement, and expectations-setting.
The group explored the need for and language by which article submissions in the form of abstracts, acceptances, and rejections could be vetted and communicated. The issue of reviewers was also discussed as a means by which the Workgroup could distribute its submission load and cultivate potential workgroup members as needed.
During the workshop, we mapped out what this experiment in crowd-sourced knowledge plus peer-review would look like in VA.
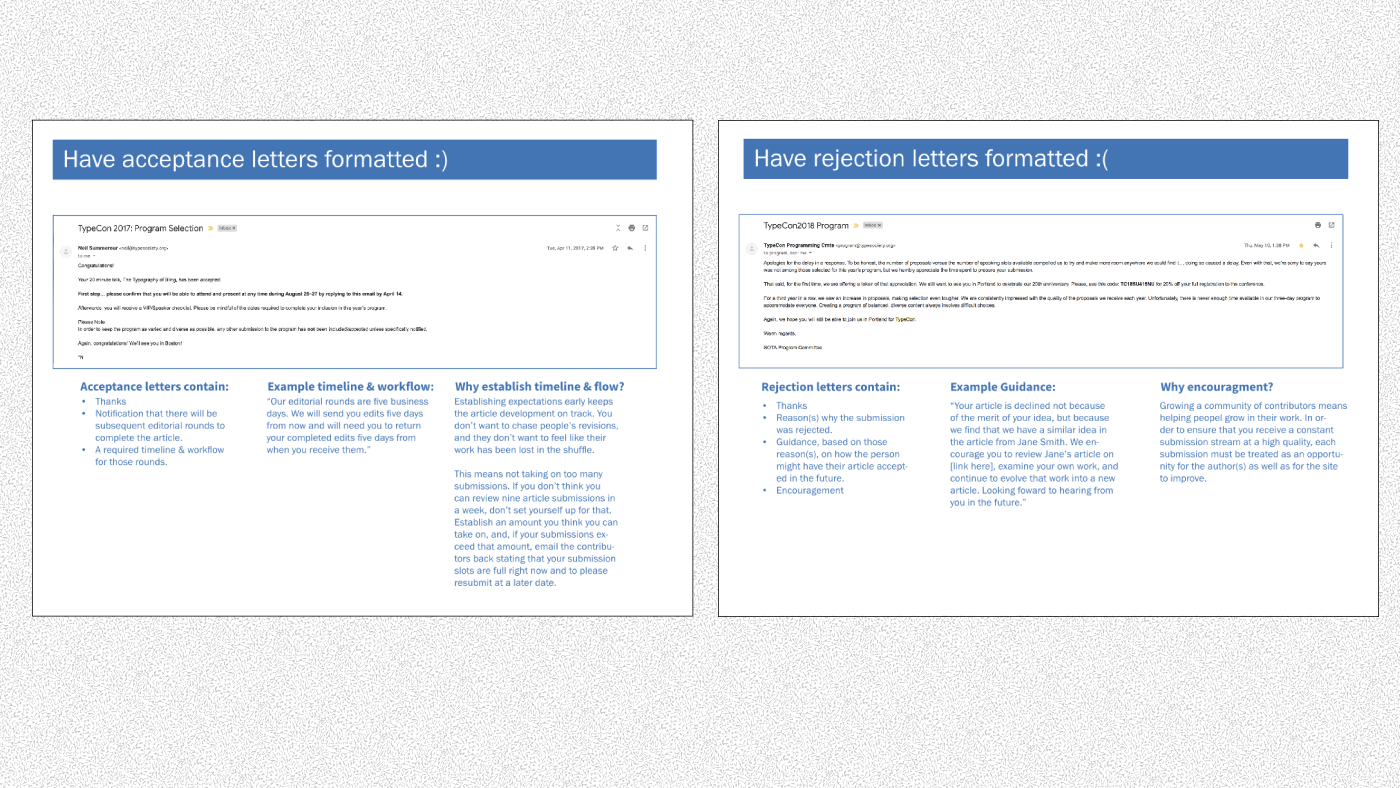
Similar to providing the scripts in the Welcome to Telehealth project, we prototyped what might be needed to work with people who make submissions to provide edits for successful submissions and, when necessary, provide helpful rejections that direct people who to improve their submissions.
Prioritization of Telehealth Toolkit Site Categories
To support the development of the site, we also established the categorial order for site development. This allowed the Editorial Working Group to request and receive submissions at a realistic pace.
These categories were gathered from the field research and were based on instructional materials developed by facilities. In order of development prioritization, they were
- Getting Providers Started Includes topics such as: Understanding Provider Needs, One-on-One Training, Talent Management System, etc.
- Telehealth Staff Training Includes topics such as: Identifying Veteran Candidates, Parameters for Telehealth Appointments
- Best Practices Includes examples of best practice
- Resources Includes topics such as: Technical Support, Forms and Templates, Contacts, etc.
- Frequently Asked Questions Includes topics such as: General Questions and Statistical Benefits
- Telehealth Experience Includes topics such as: Veteran Stories, Overcoming Challenges, Tips for Appointments, History of Telehealth
- Marketing Includes topics such as: National Announcements, Digital Posters, Print Posters and Brochures
- Telehealth Program Includes topics such as: VVC, CVT, Home Telehealth, Store and Forward and Apps
Project Conclusion
Shortly after this workshop, Telehealth took the project over for their continued development. Unfortunately, this means that I'm not sure how the Editorial Working Group is doing today. Given the proliferation of knowledge-sharing list serves and Knowledge Management Summits I have attended, I feel certain that this crowd-sourced, peer-reviewed model will come back into my orbit soon.